COVID-19: Updates and Resources
American Society of Retina Specialists (ASRS) Member Alert Regarding the COVID-19 Pandemic
*5/6/2020: This alert is being updated regularly
(Bolded areas below reflect updated information)
Background
The COVID -19 pandemic has challenged the health care infrastructure worldwide. All specialties of medicine are impacted. The field of ophthalmology has responded with guidance from the American Academy of Ophthalmology (AAO). Please refer to the AAO and Centers for Disease Control (CDC) for daily updates on the spread of the virus and the best evidence regarding transmission and containment. This ASRS report is to provide guidance to retina specialists regarding issues unique to our specialty in both the clinic and operating room.
Clinic
In accordance with guidelines from many state health departments, the AAO and the US Surgeon general’s warning, the clinic should be restricted to essential patient visits only. Such visits that may be considered essential include: new emergency patients, patients receiving intravitreal injection therapy and early postoperative follow-up patients. For new emergency patients, extra steps in the telephone triage process should be made to ensure that the patient is not at high risk of COVID-19 infection including travel to high risk areas, contact with known or suspected COVID-19 patients or symptoms of viral infection including fever, cough or shortness of breath. Prior to entering the clinic, signage should be posted asking patients not to enter if they have symptoms or are at high risk of infection through exposure or travel. Click for example of a sign.
When possible, the patient should enter the clinic alone and those accompanying the patient should be encouraged to remain outside the clinic during the patient visit unless their presence is absolutely necessary. Patient time in the office should be minimized and waiting areas set up to distance people from each other by 3-6 feet if possible. Consider taking cell phone numbers and having patients wait outside of the clinic until they can be seen. Consider injection only visits without dilation or extensive examination for patients receiving treatment on a scheduled basis who have no interval changes noted in symptoms or visual acuity. In the event that a patient with symptoms of or exposure to COVID-19 infection enters the clinic, they should be isolated from other patients and staff. This patient should then be further assessed by a physician or designee to determine the proper disposition.
The retina specialty is unique in ophthalmology in that a significant percentage of clinic visits involve an intravitreal injection without which the patient is at risk for permanent vision loss. Patients most commonly in need of injection therapy are also at greatest risk of morbidity and mortality from the COVID-19 infection including the elderly and those with a compromised immune system, particularly patients with diabetes. It is important when determining whether an upcoming patient visit is essential, the retina specialist weigh the risk of infection exposure against the risk of vision loss without treatment. This determination will vary by region and over time based on the local prevalence of infection.
When examining and treating patients deemed to be low risk for COVID-19 infection or exposure, the current recommendation is to employ standard (universal) precautions. As with other respiratory viruses, transmission is primarily due to respiratory droplets produced when an infected person coughs or sneezes. Because the examination and treatment of retinal conditions is done face to face and patients with COVID-19 can be asymptomatic carriers, the practitioner should do all they can to minimize the risk of droplet transmission. Slit lamp shields and facemasks should be considered. Patients felt to be at high risk for exposure or with known COVID-19 infection should be evaluated in a controlled hospital setting and current hospital protocols should be followed.
In the situation where a proven COVID-19 patient has been in the clinic, personnel who have been significantly exposed should self-quarantine and the local health department should be immediately notified for further action and guidance. The most up-to-date guidance for risk assessment and management of healthcare personnel potentially exposed to COVID-19 can be found here.
In certain circumstances, it may be determined that injection therapy would be best delivered outside of the clinic and in the patient’s living facility. Centers for Medicare and Medicaid Services (CMS) restrictions for home visits have been reduced. It is no longer necessary to document the need for medical necessity of a home visit. Physicians that are practicing within their scope and are already credentialed with CMS are authorized to perform home visits. The codes listed below should be used instead of the in-office E/M or Eye Codes normally used. The POS (place of service) designation is 12 instead of 11. CMS also reports that claims with 67028 and J9035/J2778/J0178/J0179 will pay when using POS 12. It is important that each provider confirm this information with their local carrier.
|
Code |
Description |
|
99341 |
NP – LOW SEVERITY – 20 MIN |
|
99342 |
NP – MODERATE SEVERITY – 30 MIN |
|
99343 |
NP – MODERATE TO HIGH SEVERITY – 45 MIN |
|
99344 |
NP – HIGH SEVEIRTY – 60 MIN |
|
99345 |
NP – PT UNSTABLE OR SIGNIFICANT NEW PROBLEM – 75 MIN |
|
|
|
|
99347 |
EP – SELF-LIMITED OR MINOR – 15 MIN |
|
99348 |
EP – LOW TO MODERATE – 25 MIN |
|
99349 |
EP – MODERATE TO HIGH – 40 MIN |
|
99350 |
EP – PATIENT UNSTABLE OR NEW PROBLEM – 60 MIN |
Telemedicine
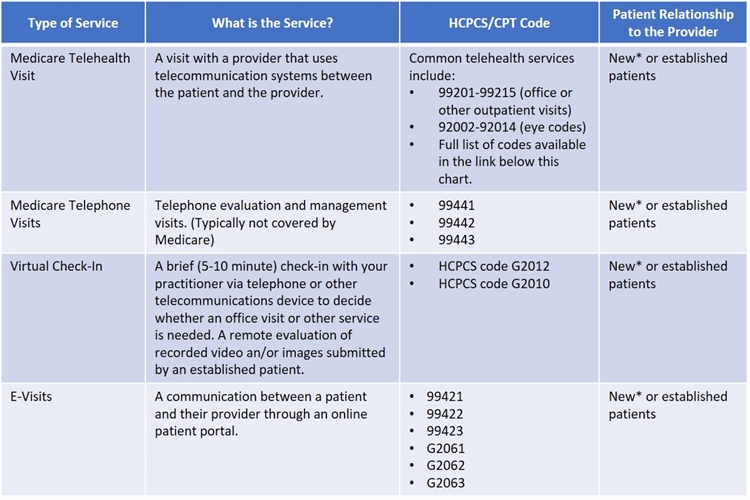
Telemedicine and home-monitoring devices may be used in lieu of face-to-face examinations in certain circumstances. Guidance is available from the AAO, CMS and the AMA. During the COVID-19 emergency, the federal government has expanded telehealth benefits for Medicare beneficiaries, including allowing services for both new and established patients and paying for telephone E/M services similar to office and outpatient visits as if they were performed in person. A chart outlining telemedicine services is below and here is a summary of expanded COVID policies.
*To the extent that the 1135 waiver (during COVID-19) requires an existing relationship, HHS will not conduct audits to determine if the relationship exists.
Here's a complete list of common telehealth services: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
Operating Room
Based on guidance from the American College of Surgeons, as of March 18, 2020, the AAO recommends that all elective surgery be postponed until at least April 6, 2020. There is, however, no guidance on what ophthalmic procedures are elective or not. It is important to identify those retinal surgery indications that, if not done in a certain timeframe, will result in severe vision loss. Such designations include: 1) Emergent, 2) Urgent, and 3) Non-urgent, non-elective. Examples of emergent/urgent indications are listed below. For emergent surgical indications, the risk of permanent vision loss without early intervention is high and access to the operating room is vital. For urgent surgical indications, the risk of severe and permanent vision loss without immediate surgery is not as high and treatment can be delayed. It is important that the retinal surgeon have discretion as an urgent situation can become emergent. For the non-urgent, non-elective indications, surgery can be delayed without significant risk to further vision loss. It is possible that, in following non-urgent, non-elective patients that their condition can worsen and the urgency increase. It is important that retina specialists are judicious with their use of the emergent and urgent designations. Many factors must be considered in assessing the need for and urgency of surgery and strict guidelines cannot be made.
Retina Emergent/Urgent Procedures
*Note: List is directed toward OR/ASC/HOSPITAL administration to inform decisions on OR time allocation.
Procedure |
Diagnostic Indication |
|
Vitrectomy (MIVS)/Scleral Buckle |
Retinal Detachment/Trauma/Intraocular Infection/Vitreous Hemorrhage/Retinal Tear/Intraocular Foreign Body |
|
Membrane Peeling/ILM peeling |
Proliferative Diabetic Retinopathy/Proliferative Vitreoretinopathy/Complex preretinal Membrane/Complex macular pathology or hole |
|
Pars Plana Lensectomy/Phacoemulsification |
Lens Complications Acute |
|
Repair Open Globe |
Trauma |
|
Examination under Anesthesia (EUA) |
Pediatric/Developmentally Delayed Evaluation |
|
Laser Indirect Retinopexy – Complex |
Retinal Detachment/Retinal Tear/Trauma |
|
Pneumatic Retinopexy |
Retinal Detachment |
|
Enucleation |
Trauma/Infection/Intraocular Malignancy |
|
Ocular Brachytherapy |
Intraocular Malignancy |
Conclusion
In this unprecedented time, it is more important than ever that retina specialists do everything possible to minimize risk of disease transmission to our patients and our staff while treating and preventing vision loss. Please keep up-to-date with guidance from the ASRS, AAO, CDC, WHO as well as state and local health agencies.
Resources
ASRS Resources
- ASRS Analysis of the CARES Act
- ASRS PHE Telehealth Guidelines
- ASRS List of Emergent/Urgent OR Procedures
(List is directed toward OR/ASC/HOSPITAL administration to inform decisions on OR time allocation) - Example: Justification for Essential Procedure Form
(*Note this example is specific to the state of Florida) - Guidance for Patients
- Small Business Owner's Guide to the CARES Act
- COVID-19 Business Information
- Economic Injury Disaster Loan
- Paycheck Protection Program