Polypoidal Choroidal Vasculopathy

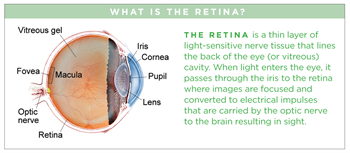
Polypoidal choroidal vasculopathy (PCV) is a disease primarily affecting the vascular layer of blood vessels in the choroid (pronounced CORE oid), resulting in damage to the overlying retina where the photoreceptor cells responsible for vision reside (see illustration).
Symptoms
Patients with PCV often experience blurred vision or a blind spot in (or near) the center of their vision in one or both eyes. These symptoms may appear suddenly and tend not to vary throughout the day. Your retina specialist may even diagnose PCV early before it has caused any symptoms.
Causes
PCV is characterized by abnormally shaped vessels in the choroid, but the precise causes of PCV remain a mystery.
We know that PCV:
- Tends to occur in individuals over the age of 60 (but may occur much younger)
- Affects those of Asian and African descent more than Caucasians
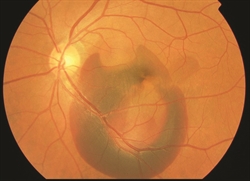
- Shares some clinical features with wet age-related macular degeneration The abnormal vessels in PCV cause vision loss when they leak fluid or blood into or under the retina (Figure 1). The abnormal vessels in PCV may also cause scarring or loss (sometimes called atrophy) of retinal tissue. Although PCV appears to affect only one eye in some patients, it often goes on to affect both eyes over time, so frequent monitoring is important.
Diagnostic testing
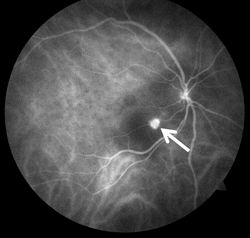
The most important test used to diagnose PCV is a careful dilated eye examination by your retina specialist. In addition, fluorescein and indocyanine green (ICG) angiography may be useful (Figure 2). These 2 tests are able to create detailed images of the retinal and choroidal blood vessels, which can assist your retina specialist in identifying important abnormalities.
Both tests require a special dye to be injected into a vein (usually in the arm or hand) before retinal photographs are taken. Optical coherence tomography (OCT) scanning of the retina is also routinely used to aid in diagnosis of PCV.
Treatment and prognosis
Unfortunately, some patients with PCV experience irreversible central vision loss in one or both eyes. Early diagnosis and treatment, however, may restore vision and prevent further vision loss in some patients. The most common treatments for PCV are intravitreal (in-the-eye) injections of an anti-VEGF medication and photodynamic therapy (PDT).
Vascular endothelial growth factor (VEGF) is a molecule generated by the body that causes the abnormal vessels in PCV to leak fluid and to bleed into and under the retina. Injections of anti-VEGF drugs into the eye block the activity of VEGF and often result in a decrease in the fluid or blood caused by the abnormal vessels.
Successful treatment of PVC often requires repeat dosing of anti-VEGF medication as frequently as every 4-6 weeks to prevent increased leakage or bleeding. In photodynamic therapy (PDT), an intravenous infusion of a special photosensitizing medication (verteporfin) is injected over 10 minutes; this makes the eye more sensitive to light. Then a cold laser is applied to the retina and choroid to damage or destroy the abnormal blood vessels found in PCV.
On rare occasions, surgical vitrectomy (a procedure to remove the eye’s vitreous gel) may be used to remove or displace a large hemorrhage caused by PCV