What is Diabetic Retinopathy?
Diabetic retinopathy is a complication of diabetes that causes damage to the blood vessels of the retina—the light-sensitive tissue that lines the back part of the eye, allowing you to see fine detail.
It is the most common cause of irreversible blindness in working-age Americans. Diabetic retinopathy occurs in more than half of people who develop diabetes.
The Retina and Diabetic Retinopathy
The retina is a thin layer of light-sensitive nerve tissue that lines the back of the eye cavity.
When light enters the eye, it passes through the iris to the retina where images are focused and are converted into electrical impulses that travel through the optic nerve to the brain resulting in sight.
Watch What is a Retina to learn more.
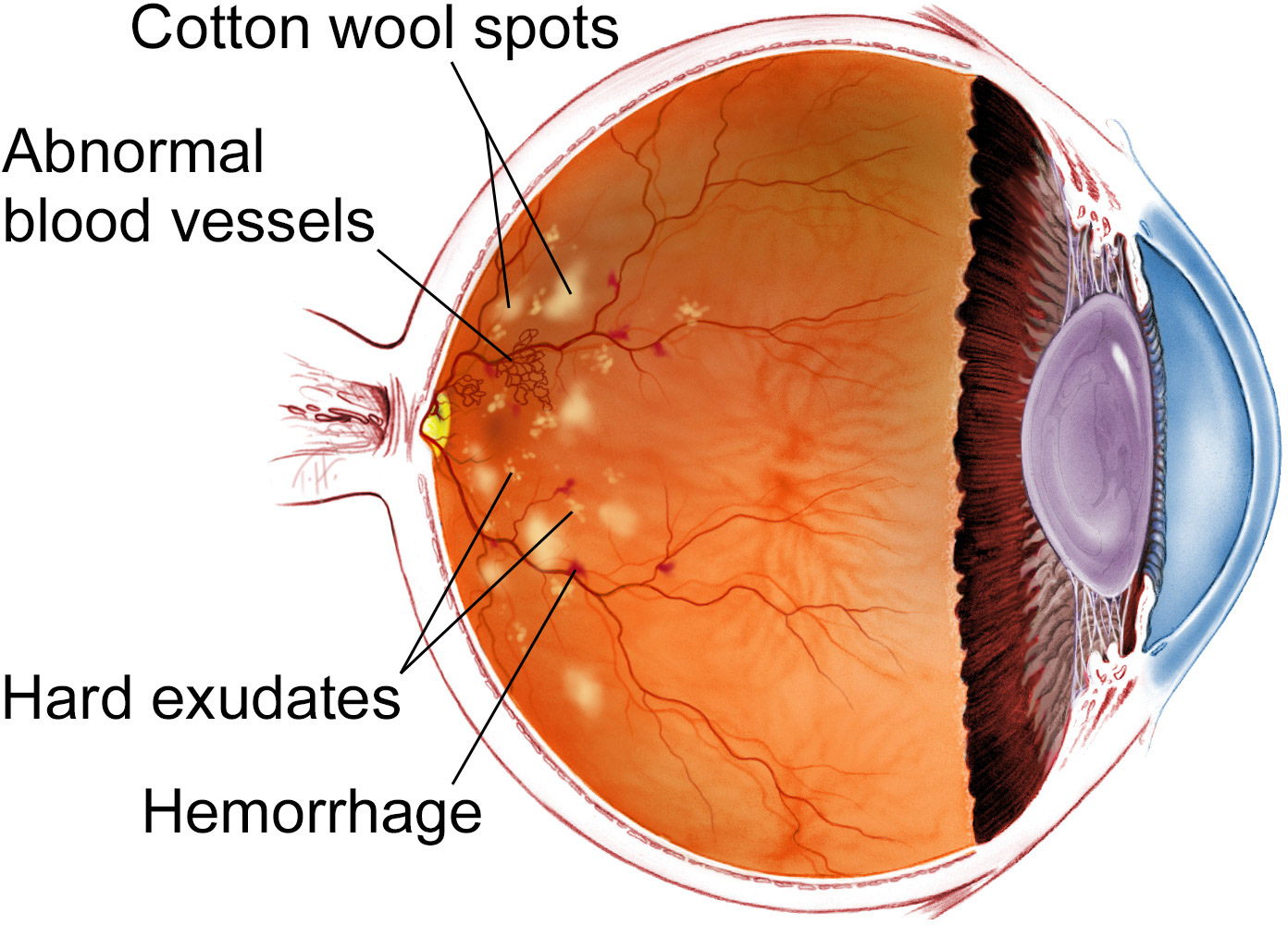
With diabetic retinopathy, elevated sugar levels from diabetes can damage the small blood vessels that nourish the retina and may, in some cases, block them completely. When damaged blood vessels leak fluid into the retina it can cause swelling, poor circulation and scarring leading to vision loss.
Who is at risk?
Anyone who has diabetes—including Type 1 (also referred to as juvenile diabetes), Type 2 (also referred to as adult-onset diabetes) and gestational diabetes—is at risk of developing diabetic retinopathy.
Additional factors can increase the risk:
- Disease duration: the longer you have diabetes, the greater the risk of developing diabetic retinopathy
- Poor control of blood sugar levels over time
- Hypertension (high blood pressure)
- Kidney disease
- High cholesterol levels
- Pregnancy
- Typical age at onset for people with Type 1 diabetes: 5–14
- Typical age at onset for people with Type 2 diabetes: 40–60
What are the symptoms?
You may have diabetic retinopathy for a long time without noticing symptoms, and at that point substantial damage may have occurred.
Symptoms you may notice in one or both eyes include:
- Blurred or distorted vision
- Difficulty reading
- The appearance of spots—commonly called “floaters”—in your vision
- A shadow across the field of vision
- Eye pressure
- Difficulty with color perception
If you experience any of these symptoms, see a retina specialist as soon as possible.
What can be done to prevent it?
Patients with diabetes frequently ask, “Is there anything I can do to keep from getting diabetic retinopathy or to prevent or treat vision loss once it occurs?”
If you have diabetes, the National Eye Institute suggests that you keep your health on TRACK:
Take your medications as prescribed by your doctor
Reach and maintain a healthy weight
Add physical activity to your day
Control your ABCs—A1C, blood pressure and cholesterol levels
Kick the smoking habit
Regular dilated retina exams can reduce the risk of developing more severe complications from the disease.
If you have diabetes, it is extremely important to maintain the eye examination schedule put in place by your retina specialist. How often an examination is needed depends on the severity of your disease. Through early detection, the retina specialist can begin a treatment regimen to help you prevent vision loss and preserve the activities you most enjoy.
How is it diagnosed?
The best way to diagnose diabetic retinopathy is a dilated retina exam. During this exam, the physician places drops in the eyes to make the pupils dilate (open widely) to allow a better view of the inside of the eye, especially the retinal tissue.
The physician will look for:
- Swelling in the retina that threatens vision (diabetic macular edema)
- Evidence of poor retina blood vessel circulation (retinal ischemia—pronounced iss KEY me uh)
- Abnormal blood vessels that may predict an increased risk of developing new blood vessels
- New blood vessels or scar tissue on the surface of the retina (proliferative diabetic retinopathy)
If you are over age 50, a dilated retina exam every 1 to 2 years is a good idea so that a physician can look for signs of diabetes or diabetic retinopathy before any vision loss has occurred.
In addition to this exam, physicians use other advanced tests to detect and manage diabetic retinopathy.
What are the treatments?
There are many approved treatments for diabetic retinopathy, including intravitreal (in-the-eye) injections, laser treatments and surgery. These procedures can be done in an office or hospital setting to prevent, treat or reverse damage from diabetes in the retina.
Early diagnosis and treatment are very important in order to preserve sight and can virtually eliminate vision loss. For those who do experience vision loss from diabetic retinopathy, there are resources that can help. For example, your retina specialist may recommend a low vision rehabilitation program to make everyday living with this disease a little bit easier.