
Choroidal Detachment
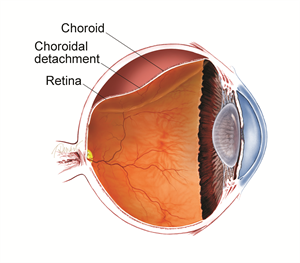
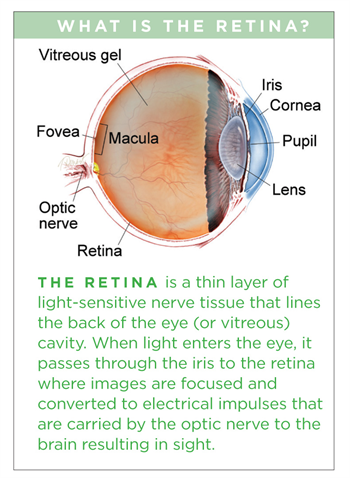
The choroid (pronounced “CORE-oyd”) is a spongy layer of blood vessels that lines the back wall of the eye between the retina and the sclera (or the white part of the eye). It plays an important role in delivering oxygen and nutrients to the outer half of the retina. The choroid is normally directly next to the sclera, but can be displaced by fluid or blood, leading to a choroidal detachment (separation).
PDF Fact Sheet LARGE-PRINT VERSION Spanish Translation Chinese Translation
Symptoms
When the choroid is detached from the back wall of the eye, patients may not feel anything at all, or may feel that the eye is achy and sore. In some cases, a choroidal detachment can cause more severe pain. Often, the vision is blurred as well, though the degree of blurring varies and often relates to other eye issues that can accompany a choroidal detachment, such as recent surgery, or high or low pressure in the eye (intraocular pressure).
Causes
In general, choroidal detachments can be categorized as “serous” (fluid filled), or “hemorrhagic” (blood filled). Serous choroidal detachments are typically associated with a low pressure in the eye and are usually only mildly uncomfortable. In contrast, hemorrhagic choroidal detachments are commonly painful, and often associated with a high intraocular pressure. Serous choroidal detachments most commonly occur in the setting of low intraocular pressure after eye surgery. Inflammation, trauma, cancer, and certain medications can also cause a serous choroidal detachment to occur. In some patients, especially in those who are far-sighted, serous choroidal detachments can occur spontaneously.
In contrast, hemorrhagic choroidal detachments occur when a choroidal blood vessel bursts and suddenly fills the space between the choroid and the sclera with blood. This most often occurs during surgery but can occur following surgery, and is more frequent in older patients with a history of hardening of the arteries, or who use medications to thin their blood.
Some eyes with low pressure following glaucoma surgery can develop serous or hemorrhagic choroidal detachment months or years following this surgery.
Risk factors
Risk factors for developing a choroidal detachment include:
- Recent eye surgery
- Use of blood thinners (such as warfarin (Coumadin®))
- A very short eye (“nanophthalmos”)
- Eye trauma
- Inflammation in the eye
- Older age
- Atherosclerosis (plaque buildup inside the arteries)
- History of choroidal detachment in the other eye
- Glaucoma (a condition where fluid buildup in the eye causes an increase in eye pressure that damages the optic nerve)
Diagnostic testing
Your retina specialist will perform a detailed eye exam. Often, an ultrasound is helpful to document the size and composition of the choroidal detachment (serous, hemorrhagic, or mixed), and to follow the change in size over time (Figure 1).
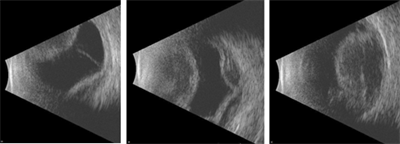
An echographic (ultrasound) image of the eye shows a choroidal detachment. Your retina specialist can use these images to differentiate a choroidal detachment from a retinal detachment, characterize the size and type of the choroidal detachment (ie serous, hemorrhagic, or mixed), and monitor changes over time.
Treatment and prognosis
Choroidal detachments are generally treated with topical medications, such as eye drops, that help reduce inflammation and dilate the pupil. Small postoperative choroidal detachments often heal on their own a few days after surgery.
In cases where the intraocular pressure is elevated, medications to lower the eye pressure are sometimes prescribed as well. In cases of serous choroidal detachments caused by persistently low pressure after surgery due to a leaking surgical incision, measures may be required to close the leak.
In some cases, choroidal detachments require surgical drainage. The timing of this surgery depends on many factors, including the status of the structures inside the eye, the pressure in the eye, and the amount of time that has passed since the choroidal detachment first occurred. The visual prognosis is more guarded in eyes with massive hemorrhagic choroidal detachments, but most eyes with choroidal detachments have a good visual prognosis, whether or not treatment is required.
