
Age-Related Macular Degeneration—Dry Forms Including Geographic Atrophy
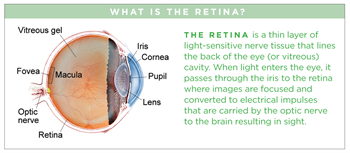
(AMD) is a deterioration of the retina (a thin layer of light- sensitive nerve tissue that lines the back of the eye) and the choroid (the layer of blood vessels and connective tissue between the retina and the white of the eye).
AMD may lead to substantial loss in visual sharpness or acuity. Yet, many people with AMD maintain reading vision throughout their lives. AMD is the leading cause of significant visual acuity loss in people over age 50 in developed countries.
Symptoms
Early stages of dry AMD may not show any symptoms. In intermediate dry-AMD stages, patients may have difficulty reading in dim light or transitioning from light to dark; they may also notice a decrease in the intensity or brightness of colors, and some early distortion (warping) of straight lines.
In the more advanced GA stage, individuals experience more marked distortion of straight lines, difficulty reading and driving at night, gradual loss of central vision, or dark, blurry areas in the center of vision.
In reticular pseudodrusen (RPD), patients also note decreased vision in dimly lit settings, and may need longer to adjust from bright light to dim light.
Causes
The exact cause of AMD is unknown, but the condition develops as the eye ages. There are 2 types of AMD: non-neovascular or dry AMD in 85% of affected individuals; and neovascular or wet AMD in 15%.
Dry AMD can be further divided into early, intermediate, and late stages. In early stages of dry AMD, small drusen—pale-yellow lesions—form beneath the retina (Figure 1A). Drusen are usually harmless, but as they accumulate, dry AMD can progress. Pigmentary changes can occur along with drusen.
Intermediate dry AMD is characterized by larger drusen (Figure 1B). Areas of atrophy or wasting also may develop in the retina; if the atrophic area is significant and has sharp borders, it constitutes the late stage of dry AMD and is termed geographic atrophy (GA).
GA most commonly starts in the region next to the center of the retina, called the fovea and is called non-central or non-foveal GA (Figure 2A). Progression of GA lesions into the fovea in foveal GA (Figure 2B) leads to loss of central vision over time.
Dry-AMD stages, especially GA, can be also associated with whitish-yellow dots connected in a reticular, or net-like pattern. These are termed reticular drusen or reticular pseudo-drusen (RPD) or subretinal drusenoid
deposits (Figure 3).

Figure 3. Whitish-yellow dots in a reticular, or net-like pattern—termed reticular drusen or reticular pseudo-drusen (RPD) or subretinal drusenoid deposits—are associated with dry-AMD stages, particularly GA. Image by Jeffrey G. Gross, MD, FASRS. Retina Image Bank; Image 1082. © American Society of Retina Specialists.
Risk factors
- Age—the strongest risk factor
- Family history of AMD
- Caucasian race
- Cigarette smoking
Possible risk factors:
- Female gender
- High cholesterol
- Lower education level
- Sunlight exposure
- Light iris color
- Low dietary fish intake
- Far-sightedness
- Cardiovascular (heart) disease
- Higher body mass index (BMI)
- Having a diet low in lutein and zeaxanthin/antioxidants
- High blood pressure
Diagnostic testing
Disease features related to AMD may be found in the retina and in the layers beneath it.
A diagnosis of dry AMD is made by a clinical examination with a slit lamp and by using several types of imaging, including:
To rule out conversion to the wet form of AMD, the following imaging studies may also be performed:
- Optical coherence tomography angiography (OCT-A)
- Fluorescein angiography (FA) and indocyanine green angiography (ICGA)
Visual function can be measured by using the patient’s ability to read letters on eye charts. Also used: a technique named microperimetry that evaluates the sharpness of the vision in certain areas of the macula, or center of the retina responsible for central vision.
Treatment and prognosis
There are two FDA-approved drugs, Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol) that help to slow geographic atrophy progression. Both drugs are injections into the vitreous cavity of the eye every one to
two months.
Also, the Age-Related Eye Disease Studies (AREDS), conducted by the National Eye Institute, have found that a nutritional supplement formula (AREDS2) may delay and prevent intermediate dry AMD from converting to wet AMD.
The AREDS2 supplement formula, which is widely available over the counter, contains specific doses of vitamins and minerals used in the AREDS2 Study:
- Vitamin C
- Lutein
- Vitamin E
- Zeaxanthin
- Zinc
- Copper
Although patients with either form of AMD can experience a progressive decrease in visual acuity, it would be very rare to lose all vision.
Following a Mediterranean-type diet (higher whole-fruit consumption, lower red-meat consumption, low to moderate alcohol use, and a higher ratio of monounsaturated fatty acid to saturated fatty acid) is associated with a lower risk of progression to large drusen and to GA, and to slower enlargement of GA.
GA patients can take advantage of low-vision therapy using assistive devices to achieve improved mobility, reading and distance viewing, and facial recognition.
The Implantable Miniature Telescope is a surgical option available to low- vision patients with GA; it enlarges objects in the center of the visual field so they can be seen by intact areas of retina surrounding GA. Importantly, investigational treatments are in late stages of development for intermediate AMD, non-foveal and foveal GA.




