Sickle Cell Retinopathy
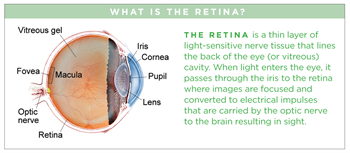
Sickle cell retinopathy is present in some patients with sickle cell disease. In sickle cell retinopathy, blockage of blood vessels in the retina and choroid (pronounced CORE-oid) results in abnormal blood vessel growth and thinning of the retina. These physical changes and their consequences can impair vision.
Symptoms
Patients with retinal involvement of sickle cell disease often do not have any eye symptoms. However, when symptoms are present, patients describe:
- Blind spots
- Sudden onset of floaters or blurred vision
- Flashes of light
- Loss of side vision or curtains
Causes
Sickle cell disease is:
- The most common inherited blood disorder
- Most often found among people of African, Hispanic, and Caribbean descent
- Caused by a mutation in the beta-globin gene, which decreases the ability of red blood cells to carry oxygen
Red blood cells carrying beta-globin mutations can become elongated and rigid, also known as sickling. These cells are more fragile and can easily be destroyed. Red blood cell sickling can block blood vessels and prevent oxygen transport to tissues, resulting in ischemia (pronounced iss KEY me ah, meaning an insufficient blood supply). Dehydration, decreased oxygen levels, and infection can all cause sickling. Symptoms of sickle cell disease commonly include painful vaso-occlusive crises, as well as pneumonia and strokes.
Each cell in the human body carries 2 beta-globin genes. The normal gene is adult hemoglobin (HbA). The 2 most common mutations causing sickle cell disease are called hemoglobin S (HbS) and hemoglobin C (HbC). The most
common combinations involving mutations are:
- HbSS disease, also known as sickle cell anemia. This causes the most severe symptoms of sickle cell disease throughout the body. Vision loss is less common in patients with HbSS disease.
- HbSC disease, a less severe form of sickle cell disease affecting the body. This form tends to affect the retina more frequently, and patients have higher rates of vision loss.
- HbAS, also known as sickle cell trait. This does not usually present with eye symptoms. However, high eye pressure and low oxygen levels in patients can rarely lead to vision loss in patients with sickle cell trait.
Given the severity of these symptoms, screening of newborn babies for sickle cell disease is now mandated in all 50 states. However, it is still important to test patients in whom sickle cell disease is suspected since they might not have been screened.
Retinal findings: Sickle cell retinopathy can affect several parts of the retina.
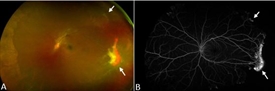
- Proliferative sickle retinopathy occurs in ischemic retina. In response to the lack of oxygen, these tissues release factors that promote blood vessel formation that impacts vision. However, these blood vessels are fragile and can cause bleeding. These vessels can also form networks that resemble a sea fan and are characteristic of sickle cell retinopathy (Figures 1A and 1B).
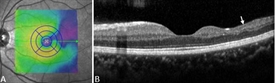
- Sickle cell maculopathy, which affects the center part of the retina, occurs when there is decreased blood flow to this part of the eye. This abnormal blood flow causes patches of retinal thinning (Figures 2A and 2B). Patients will sometimes note blind spots as a result.
- Vitreous hemorrhage, or bleeding in the center part of the eye, can occur when abnormal retinal blood vessels break.
- Retinal detachments can occur from tears in ischemic retina, or from pulling of abnormal blood vessels and scar tissue on the retina. This can cause significant vision loss.
Diagnostic testing
A yearly sickle cell retinopathy screening exam with a retina specialist is recommended starting at age 10 for
those diagnosed with sickle cell disease.
- Fluorescein angiography is used to highlight blood vessels in the retina, particularly abnormal sea fan-shaped vessels, and areas without blood flow. Ultra-widefield imaging is very helpful to show vessel changes at the edges of the retina (Figure 1B).
- Special imaging known as spectral domain optical coherence tomography shows cross sections of the retina. It is useful to identify areas of retinal thinning (Figures 2A and 2B).
- An advanced form of retinal imaging known as optical coherence tomography angiography shows changes in retinal and choroidal vessels. These include blocked and abnormal blood vessels caused by the sickle cells.
Treatment and prognosis
Treatments for sickle cell disease include:
- Stem cell therapy from matched sibling donors, which can be curative
- Red blood cell exchange transfusions, which reduce abnormal beta-globin
- Hydroxyurea, a drug that increases levels of a different type of hemoglobin that can carry oxygen and therefore decrease sickling and blockage of blood vessels
Two new medications have recently been approved by the Food and Drug Administration for sickle cell disease:
- Voxelotor inhibits red blood cell sickling and destruction
- Crizanlizumab helps to prevent blood vessel blockage
Treatment of proliferative sickle cell retinopathy:
- Observation is indicated for smaller areas of abnormal blood vessel growth since these will usually disappear without treatment.
- Laser treatment of large areas of ischemia (blood vessel blockage) can prevent the release of factors that promote abnormal blood vessels.
- Drugs that prevent new blood vessel formation can be injected into the eye in select patients.
- Surgery is indicated for vitreous hemorrhage and retinal detachment.