
Acquired Vitelliform Lesions
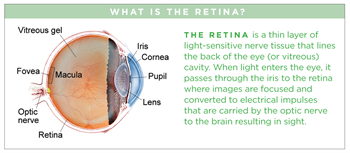
Adult-onset vitelliform maculopathy is a retinal disease characterized by round, yellowish deposits (acquired vitelliform lesions, or AVLs) found beneath the central retina or macula (Figure 1). Other names used for these findings include adult pattern dystrophy and adult-onset foveomacular pigment epithelial dystrophy.
Symptoms
Patients with adult-onset vitelliform maculopathy may notice decreased or distorted vision. In milder cases, an ophthalmologist may notice the vitelliform deposits before they have caused visual symptoms.
Causes
- AVLs usually occur in adults in their 40s and 50s. This is in contrast to the vitelliform lesions occurring in best vitelliform macular dystrophy, an inherited disorder, which usually occur earlier in life.
- AVLs are often the only abnormality seen in the eye, although they can also be associated with other yellow deposits called drusen that are considered a finding of age-related macular degeneration (AMD). (Figure 1)
- AVLs are located in the subretinal space, which is beneath the retina, but above a layer of pigmented cells known as the retinal pigment epithelium (RPE). (Figure 2)
- The deposits are thought to be primarily composed of degenerating parts of photoreceptors, the cells that make up the outer retina and are important for vision.
- Vision for patients with AVLs can vary widely, but nearly half of patients will start with and maintain vision good enough for driving (20/40 or better).
- The size of the lesions can be measured using optical coherence tomography (OCT), an imaging technique. Larger lesions (both in width and height) are associated with decreased vision. OCT can also be used to assess the outer retina by evaluating the integrity of its reflective layers.

Figure 1. A vitelliform lesion under the fovea in a right eye. The vision in this person is 20/60 with glasses. Smaller scattered yellow spots known as drusen also are visible. (Photo courtesy of K. Bailey Freund, MD) |
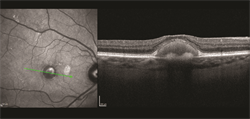
Figure 2. An infrared image (left) demonstrates the central vitelliform deposit seen in Figure 1. An optical coherence tomography (OCT) scan (right) demonstrates the vitelliform material and some thinning of the overlying outer retinal layers. The size of the deposit can be measured and tracked over time. (Photo courtesy of K. Bailey Freund, MD) |
Diagnostic testing
- A complete dilated funduscopic exam is the first step in the diagnosis of adult-onset vitelliform maculopathy. OCT is an important next step and should be repeated over time by a retinal specialist who can monitor any changes in lesion size or outer retinal integrity. (Figure 2)
- Fluorescein angiography (FA), in which a fluorescent intravenous dye is used to provide information about the integrity of retinal blood vessels and to look for signs of a possible complication of this disorder, choroidal neovascularization (the formation of new, but defective blood vessels), can also be helpful. Indocyanine green angiography (ICGA) or OCT angiography, are sometimes also used to look for choroidal neovascularization.
- Given the association between vitelliform lesions and some genetic disorders, a careful history, electrophysiologic studies, and genetic testing are sometimes indicated to help exclude the possibility of a genetic disorder leading to the eye findings.
Treatment and prognosis
It is important to differentiate AVLs from neovascular AMD, as AVLs do not require treatment with injections of anti-vascular endothelial growth factor (anti-VEGF) therapy, while neovascular AMD often does. Making this distinction can help avoid unnecessary interventions and risk associated with intravitreal treatment
- Some AVLs may resolve on their own. When they do, the resolution is often associated with atrophy, which can result in decreased central vision.
- Adult-onset vitelliform maculopathy does not affect peripheral vision
