
Endophthalmitis
is an infection inside the eye that can either be acute or chronic, meaning that it can develop very rapidly which is most common, or develop slowly and persist for long periods of time.
Download Fact Sheet Large-Print Version
Symptoms
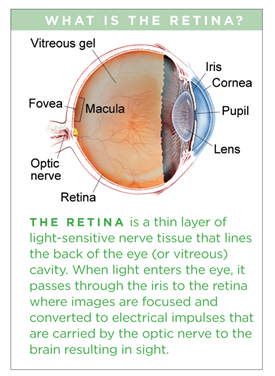
Endophthalmitis causes the white of the eye to be inflamed. There may be a white or yellow discharge on or inside the eyelid, and the cornea may show a white cloudiness. There may also be a layer of white cells (hypopyon) present within the anterior chamber of the eye between the iris and the cornea. (Figure 1) Endophthalmitis is usually a very serious problem and prompt examination by an ophthalmologist is essential to make an appropriate diagnosis and initiate treatment.
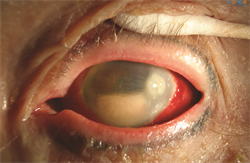
Figure 1. Hypopyon is an accumulation of white blood cells in the anterior chamber of the eye and corneal infiltrate associated with infectious endophthalmitis. Image courtesy of ©Retina Image Bank, contributed by Aleksandra V. Rachitskay, MD, Cole Eye Institute, Cleveland Clinic. 2014. Image 16250.
Other symptoms include:
- Eye pain and redness
- Decreased vision
- Trouble looking at bright lights (photophobia), usually sudden onset
Causes
Acute cases of endophthalmitis are caused by gram-positive (or less frequently gram-negative) bacteria and are most often seen within 6 weeks after surgery or trauma to the eye.
Chronic cases that occur outside of the 6-week window are often related to a previous surgery and are commonly caused by slowly progressive infections such as Propionibacterium acnes or fungus.
Finally, systemic infections can spread to the eye causing endogenous endophthalmitis. This is often associated with systemic fungal or gram-negative bacterial infections. Patients who are debilitated, septicemic (bacteria in the bloodstream), and who have weakened immune systems are particularly susceptible, especially after surgical procedures.
Risk factors
Loss of vitreous gel (also referred to as vitreous humor), disrupted posterior capsule, poor wound closure, and prolonged surgery are risk factors for developing endophthalmitis. The incidence following penetrating trauma is 4–13% and may be as high as 30% after injuries in rural settings.
Risk factors for endophthalmitis after trauma include:
- Retained intraocular foreign body (having foreign material remain in your eye following an injury)
- Delayed surgery (longer than 24 hours) to repair a full-thickness laceration
- Rural setting (soil contamination)
- Damage to the lens during trauma
Diagnostic testing
To determine what organism has caused the infection, a biopsy of the fluid within your eye needs to be obtained. This fluid is then sent to the laboratory for a determination and to decide on the best treatment.
Treatment and prognosis
In acute cases, treating endophthalmitis is an emergency and needs to be performed as soon as possible. The procedure performed will depend on your vision. If your vision is very poor, you will need to undergo an emergency surgery called a vitrectomy to remove the infectious debris from your eye and to inject antibiotics or antifungal agents directly inside your eye. Cases with better vision may only require an injection of antibiotics or antifungal agents in the office. In rare cases, only antibiotic eye drops are required.
The prognosis depends on the cause, duration, and type of organism that caused the infection. Outcomes are often less favorable for traumatic cases involving gram negative organisms. Some cases involving gram positive bacterial infections after cataract surgery fare better. Eyes with endophthalmitis often require frequent examinations to obtain the best outcomes.
